January 11, 2024
1 minute read
Important points:
- After implementation of the individualized protocol, fewer patients were prescribed opioids upon discharge.
- No patients required readmission or additional opioid prescriptions.
Researchers reported that using a personalized protocol for prescribing opioids after cesarean section reduced the number of opioids prescribed at discharge, without impacting readmissions or the need for emergency prescriptions.
“Studies have shown that patients were prescribed the same morphine equivalent dose after cesarean section, regardless of objective and subjective measures of pain before discharge.” Chinonier S. Dr. Imo, resident in obstetrics and gynecology at Parkland Health in Dallas; writes a colleague. “Furthermore, most patients do not use all of the opioids prescribed at the time of discharge. Therefore, this practice of prescribing a standard number of opioid pills, regardless of their use within the hospital, It’s leading to an overabundance of opioids.”
Imo et al. conducted a prospective cohort study; Journal of the American College of Obstetricians and Gynecologists, included data from 367 women who had previously undergone a cesarean section and 412 women who had a cesarean section after implementing personalized opioid prescribing practices at discharge. Prior to implementation, the woman was prescribed her 30 acetaminophen-codeine 300 mg/30 mg tablets. Those who underwent a caesarean section after the procedure were given ibuprofen and acetaminophen as scheduled, as well as oxycodone tablets equivalent to five times the morphine equivalent used in the 24 hours before discharge.
The primary outcome was morphine equivalents prescribed at discharge.
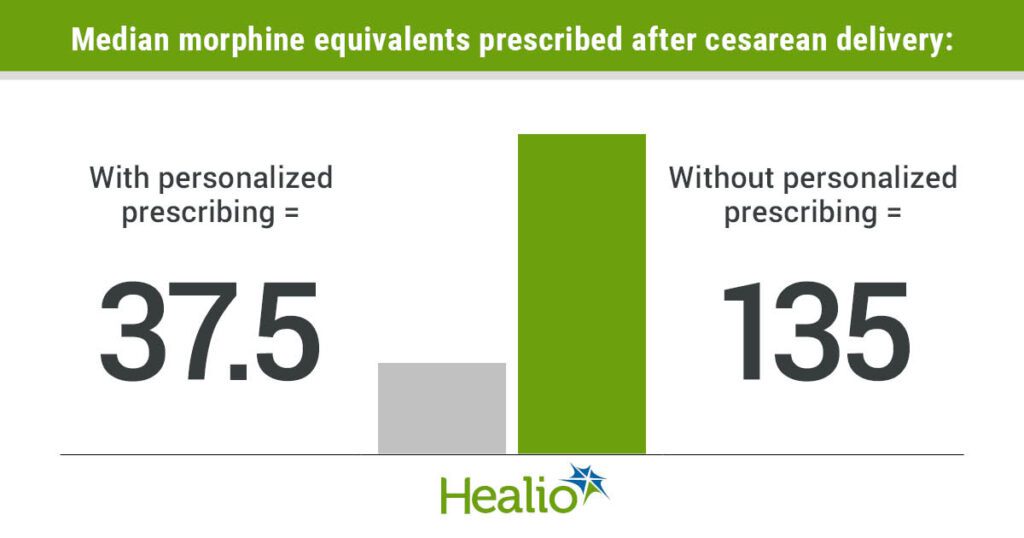
With personalized prescribing technology, the median morphine equivalent dose prescribed at discharge decreased compared to pre-introduction (37.5 vs. 135; P < .001). Researchers observed that 43% of women who had a caesarean section had no opioid prescription at hospital discharge after the procedure compared to before (all 367 patients were prescribed an opioid) did(P < .001).
The researchers noted that although there were nine hotline calls to the hospital, none required additional opioid prescriptions after a 24-hour trial in which prescribed ibuprofen was scheduled.
Overall, 2.7% of women presented to the emergency department for pain evaluation, but none required readmission or outpatient opioid prescription.
“As health care providers seek to reduce the amount of opioids they prescribe, this change in practice at a single facility will result in more than 90,000 fewer opioids being released into our community annually, with no apparent adverse effects. “This is likely to be the case,” the researchers wrote. “If implemented at a national level, the impact would be significant.”