Recent 6 children die in Ontario and 4 children in British Columbia Infectious diseases caused by bacterial infections are attracting the attention of parents. Doctors say severe cases of invasive group A streptococcal infections are extremely rare. Here’s what you need to know about the disease, which is occurring in record numbers this season and puts adults, especially those over 65, at risk.
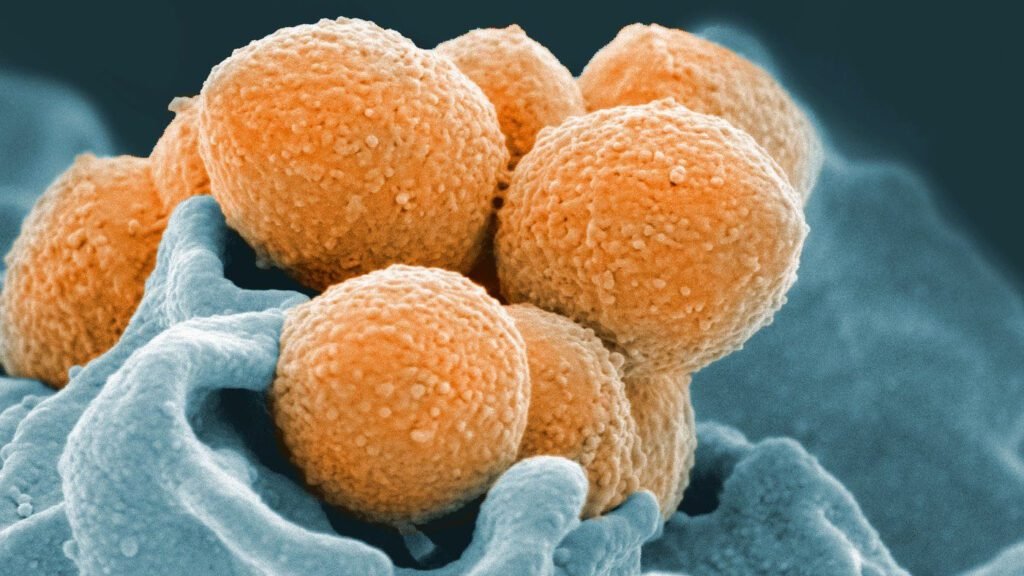
What is Group A Streptococcus?
Streptococcus is commonly found in the throat and skin. Dr. Monica Knauss, medical director of immunization programs and vaccine-preventable diseases at the B.C. Center for Disease Control, says some people don’t have any symptoms, but others get a mild case of strep throat, which is often accompanied by a fever. He said there are some. It either resolves on its own within a few days or is treated with antibiotics. A sore throat, on the other hand, is usually accompanied by a cough, runny nose, or other cold-like symptoms.
How do people get invasive group A streptococcal infections (iGAS)?
The disease becomes invasive, with bacteria entering the bloodstream and deep tissues, sometimes through wounds and the nose and throat. Knauss said the virus is transmitted through secretions from these membranes or through direct contact with infected skin lesions.
How can I prevent infection?
Washing your hands, especially before cooking or eating, is a preventive measure, as is keeping cuts and wounds clean and watching for redness or other signs of infection. It’s also important to stay home when you’re sick and get vaccinated against influenza and COVID-19.
Knauss said even a paper cut could lead to infection.
“I don’t mean to scare anyone, but it doesn’t have to be deeply traumatic. Strep infections can be caused by what’s called blunt trauma, which means the skin isn’t even punctured. However, the microorganisms were on the skin and entered the body.”
Viral infections such as influenza can cause streptococcal type A bacteria to enter the body, and these infections are more common during the winter months.
In British Columbia, 60 people under the age of 20 are infected with invasive disease, compared to thousands of people infected with influenza and respiratory syncytial virus (RSV), which can affect young children and the elderly. Highly sexual.
What should parents be careful about?
“There’s a fine line between a kid who has a fever with the flu and is miserable on the first or second day and a kid who’s having trouble,” Knauss said.
However, parents should be on the lookout for a lingering fever, difficulty breathing, a sandpaper-red rash, or a swollen tongue, sometimes called strawberry tongue. You should also be concerned about children who are groggy and have trouble waking up.
Children with worsening conditions may also have pneumococcal disease, but children are vaccinated starting at 2 months of age.
Although there is no vaccine for invasive group A streptococcus, Knauss urged parents to at least get their children vaccinated against influenza and COVID-19.
“While these infections can be prevented, they can be precursors to more serious bacterial infections.”
Who is most at risk?
Dr. Upton Allen, director of infectious diseases at Toronto’s Hospital for Sick Children, said people with weakened immune systems are most susceptible to infection. He said children between the ages of five and nine and adults over 65 are getting sick in Ontario.
“Among adults, those with long-term illnesses such as cancer, diabetes or kidney disease, or who take special medications such as corticosteroids, may be at higher risk,” Allen said. Stated. “While some of these infections may be mild, others can have serious consequences.”
He said families should be aware that lesions caused by chickenpox can be contagious and cause a Step A infection, and urged parents to ensure their children receive regular vaccinations.
“Certainly, we have had concerns throughout the COVID-19 pandemic, and we all need to advocate for strong efforts to ensure vaccines are up to date.”
What is a serious but rare type of group A streptococcus?
In very rare cases, group A streptococcus can cause necrotizing fasciitis, a flesh-eating disease. Meningitis; cerebrospinal infection; toxic shock syndrome that causes multiple organ failure. Hypotension and renal failure.
None of the four children who died in British Columbia are believed to have developed these symptoms, Knauss said.