October 23, 2023
1 minute read
Important points:
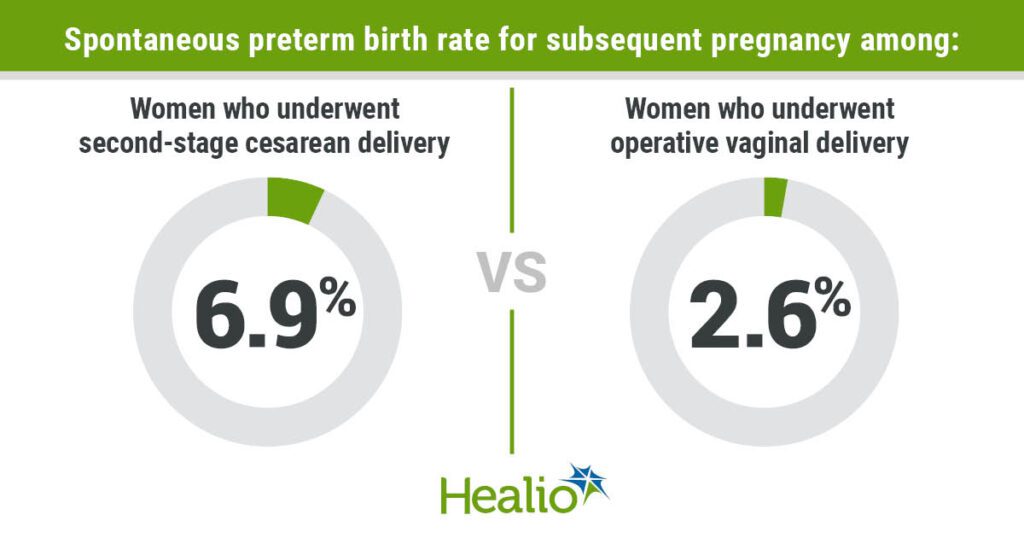
- Spontaneous preterm birth rates were higher after second-stage cesarean section compared with vaginal delivery.
- A second-stage caesarean section doubles the risk of spontaneous preterm birth compared to a vaginal birth.
A systematic review and meta-analysis shows that if a mother undergoes a second-stage caesarean delivery with a fully dilated cervix, there may be an increased risk of subsequent spontaneous preterm birth compared with a vaginal delivery.
“Given the observed association between second-stage caesarean section and subsequent preterm birth, increasing the use of operative vaginal delivery may have the potential to reduce the excess risk of preterm birth.” Dr. Abhirami Kirvarajan, master’s degree, 2nd year of residence Department of Obstetrics and Gynecology, McMaster University, Hamilton, Ontario, Canada; writes a colleague. “The association with second-stage caesarean section is concerning because second-stage caesarean section rates are increasing in some settings as operative vaginal births decline.”
Kirubarajan et al searched multiple databases for this systematic review and meta-analysis. Journal of the American College of Obstetricians and GynecologistsThe authors identified 18 retrospective cohort studies that included 605,138 women who underwent a second-stage cesarean or operative vaginal delivery and reported preterm birth rates in subsequent pregnancies.
After second-stage cesarean delivery, the combined spontaneous preterm birth rate in subsequent pregnancies was 6.9% compared with 2.6% after operative vaginal delivery.
In seven studies comparing the two, the authors observed that the risk of spontaneous preterm birth with second-stage cesarean section was twice as high as with operative vaginal delivery (OR = 2.01; 95% CI, 1.57-2.58). These studies also demonstrated that the spontaneous preterm birth rate was 5.2% with second-stage cesarean section compared with 3% with operative vaginal delivery.
According to the authors, most studies do not include important confounders and fail to address misclassification of exposure due to failed operative vaginal births, and operative vaginal births are limited by forceps and vacuum. It is said that it was thought to be a homogeneous category with no distinction.
“If a patient is concerned about multiple pregnancies, it may be beneficial to debrief with the patient after operative delivery about the potential association with subsequent increased preterm birth,” the authors write. “Screen cervical length in these patients with transvaginal ultrasound in subsequent pregnancies, especially as there is a growing trend to universally screen cervical length in the second trimester for all pregnancies. There may also be benefits to that.”